Content:
1. Introduction to a bone metabolism
2. Bone remodeling
3. Regulation of bone metabolism
4. Biochemical markers of bone metabolism
5. Selected bone diseases
_
Introduction to bone metabolism
Bones perform many functions in a human body:
1) A mechanical function – bones provide a support for muscles and protect a bone marrow
2) A reservoir of calcium and phosphates – bones influence the metabolism of calcium and phosphates significantly
3) A buffer of the 3rd line – bones release phosphate and bicarbonate in the long-term metabolic acidosis
Composition of bone
1) Cells
a) Osteoblasts and osteocytes synthesize new bone tissue
b) Osteoclasts are bone-degrading cells
2) Extracellular matrix
a) Organic component: collagen type I and non-collagenous proteins (e.g. osteocalcin, protein S)
b) Inorganic component: apatite – crystallic form Ca3(PO4)2 (it can exist in a form of hydroxyapatite – Ca10(PO4)6(OH)2, carbonate apatite – Ca10(PO4)6CO3 or fluorapatite – Ca10(PO4)6F2)
Osteoblasts
Osteoblasts originate from mesenchymal cells of bone marrow. They exhibit high proteosynthetic activity and are rich in alkaline phosphatase. Their membranes contain receptors for PTH, calcitriol, growth factors, estrogens etc. and also mechanoreceptors. Their primary function is bone matter formation, bone mineralization and management of maturation and activity of osteoclasts.
Osteoclasts
Osteoclasts are formed from hematopoietic cells (monocyte macrophage lineage). They contain lysosomes filled proteolytic enzymes (collagenase, gelatinase, cathepsins) and acid phosphatase isoenzyme. Membrane of osteoclasts contains a proton pump (it is able to decrease pH = 7 to pH = 4) and selected receptors (e.g. for calcitonin). Osteoclast activity but at the same time is controlled by signals from osteoblasts. Their primary function is bone resorption (runs parallel to an increased calcemia).
_
Bone remodeling
Throughout life bone remodeling occurs continuously. It is very important because it allows the adaptation of form and organized structure of bones to biomechanical forces, maintaining the integrity of bone (repair microtraumas) and homeostasis of calcium and phosphates.
People achieve so-called peak bone mass – PBM at age 25. Followed by variable length (average of 5 years) remodeling balance, which means that bone resorption intensity is equal to the intensity of bone formation. After this period continuous loss of bone mass begins, which is approximately 0,5 % per year – bone resorption predominates over bone formation. An increased rate of bone loss occurs in women after menopause – risk of developing osteoporosis. On the contrary, obese people do not suffer a significant loss of bone tissue because their bones are more consistently loaded – a load is one of the main regulating mechanisms.
Bone remodeling cycle lasts about 4 months and can be divided into three stages:
1) An impulse – usually greater physical load, parathormone releasing
2) Bone resorption by osteoclasts
3) Formation of new bone tissue by osteoblasts
Balance remodeling is maintained by several factors:
1) A mechanical loading of the limb
2) Hormones and local factors
3) Calcium and phosphate levels in the blood
_
Regulation of bone metabolism
Bone metabolism is regulated by many systemic hormones and locally acting substances. Systemic hormones can be divided into two groups: hormones affecting the metabolism of calcium and phosphates and other systemic hormones.
Hormones affecting the metabolism of calcium and phosphates
Metabolism of calcium and phosphates is discussed in detail in Subchapter 7/6. At this point we restrict ourselves only to an information about the effect of these hormones on bone metabolism.
In the human body parathormone, calcitriol and calcitonin play a key role in the regulation of calcium and phosphate content.
1) Parathormone
Parathormone stimulates the resorption of bone by increasing the activity of osteoclasts (stimulates transformation of monocytes to osteoclasts). The result is an increased release of Ca2+ and phosphates from the bone.
2) Calcitonin
Calcitonin inhibits osteoclast activity (inhibits transformation of monocytes to osteoclasts), thereby reduces bone resorption and it results in an increased deposition of Ca2+ in bones.
3) Calcitriol (1,25-dihydroxycholecalciferol, vitamin D derivative)
Calcitriol stimulates synthesis of proteins allowing the absorption of Ca2+ and phosphates in the small intestine. Thus calcitriol ensures the availability of Ca2+ and phosphates for bone formation. Simultaneously activates osteoblasts to synthesize collagen.
Other systemic hormones
1) Estrogens
Estrogens act like calcitonin. Therefore they inhibit bone resorption – inhibit osteoclast activity through local factors.
2) Growth hormone
Growth hormone stimulates bone formation mediated through the formation of local growth factors – insulin-like growth factors (somatomedins – IGF-1 and IGF-2).
More detailed information about insulin-like growth factors in Chapter 11.
3) Insulin
Insulin increases the synthetic activity of osteoblasts. Bone loss can occur in anuntreated diabetes mellitus.
4) Glucocorticoids
Glucocorticoids reduce the formation of new bone (they inhibit proteosynthesis in osteoblasts and their differentiation).
5) Thyroid hormones
Thyroid hormones stimulate osteoclasts, activate bone remodeling. At their overproduction an osteoporosis may develop.
An overview of system control of bone metabolism
|
Hormone |
Resorption |
Formation |
| PTH |
↑ |
↑ |
| Calcitriol |
↑ |
↑ |
| Calcitonin |
↓ |
– |
| Cortisol |
↑ |
↓ |
| Growth hormone |
– |
↑ |
| T3, T4 |
↑ |
↑ |
| Insulin |
– |
↑ |
| Sex hormones |
↓ |
↓ |
_
Local factors regulating bone metabolism
1) Factors stimulating osteoblast differentiation
a) Bone morphogenic factor (BMF)
b) Insulin-like growth factor 1 (IGF-1)
c) Platelet-derived growth factor (PDGF)
d) Fibroblast growth factor (FGF)
2) Factors stimulating osteoclast differentiation
a) M-Colony stimulating factor (M-CSF)
b) Interferons (INF-γ) and interleukins (IL-1, IL-6 etc.)
Overview of local regulation of bone metabolism
|
Local mediators |
Resorption |
Formation |
| Growth factors |
↑ |
↑ |
| Factors from osteoblasts |
↓ |
↑ |
| Inflammatory cytokines |
↑ |
↓ |
Biochemical markers of bone metabolism
Many substances can be laboratory markers of bone metabolism. Secondly, these include ions – Ca2+ (total 2,25-2,75 mmol/l, ionized 1,1-1,4 mmol/l) and phosphates (0,7-1,5 mmol/l), hormones influencing bone metabolism (e. g. parathormone, calcitonin, vitamin D / calcitriol, estrogens, glucocorticoids etc.). Besides these, there are also specific markers of bone metabolism.
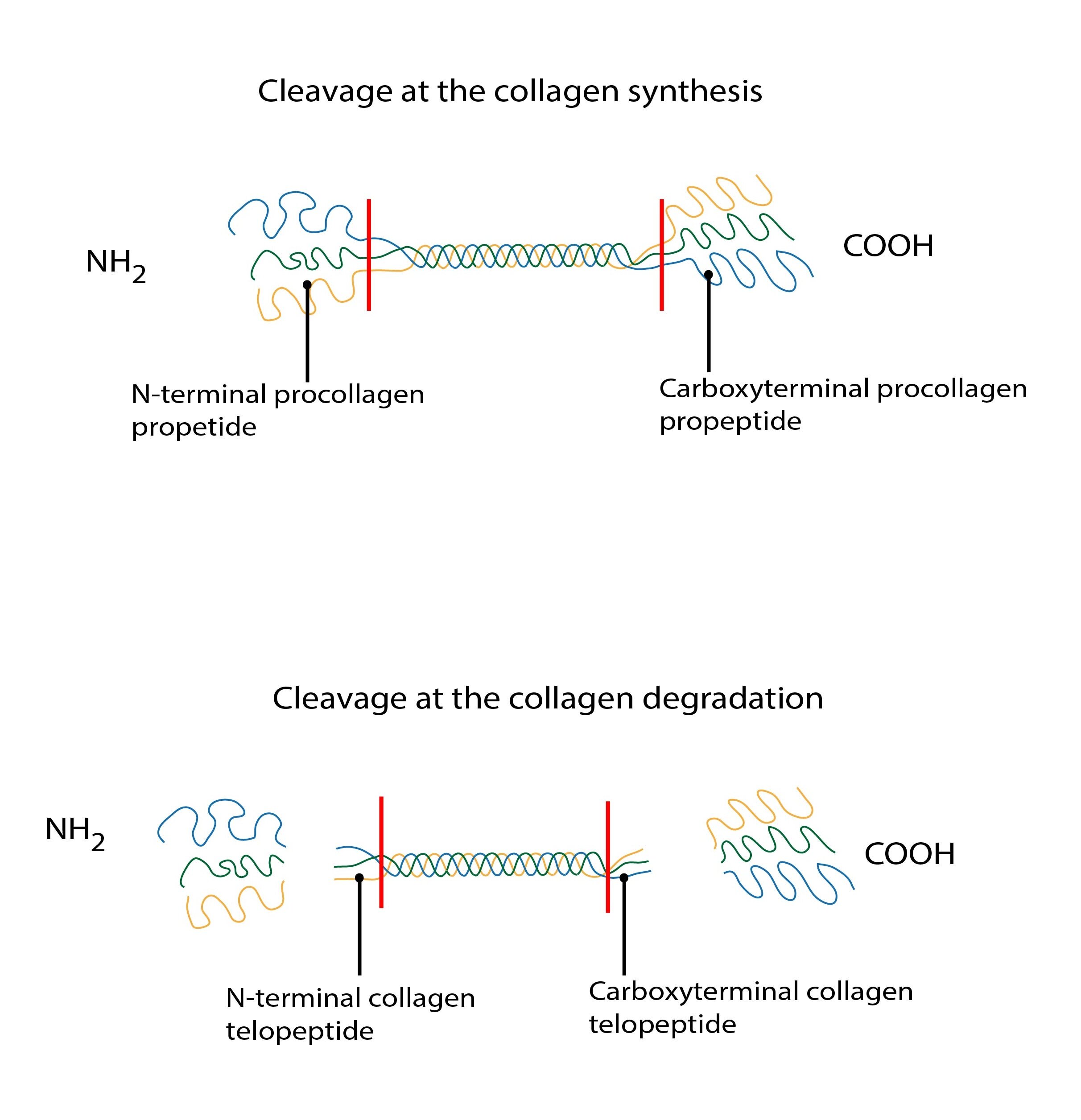
The rate of bone formation and resorption is best assessed by products generated in metabolism of organic bone matrix components (such as in the synthesis and degradation of collagen) and some enzymes. According to an elevation of these markers, they are divided into two groups – markers of bone formation and markers of bone resorption.
Markers of bone formation
Bone formation markers include: bone isoenzyme of alkaline phosphatase (ALP), terminal propeptides of procollagen type I (U-PINP, U-PICP) or serum osteocalcin.
Terminal propeptides of procollagen type I are formed by cleavage of the propeptide from procollagen.
Osteocalcin (Gla protein) is a non-collagenous bone matrix protein, its molecule contains residues of gamma-glutamic acid. Osteocalcin binds to hydroxyapatite.
Markers of bone resorption
Bone resorption markers include: bone isoenzyme of acid phosphatase (tartrate-resistant), carboxy-terminal telopeptides of collagen (U-ICTP), urinary hydroxyproline or urinary deoxypyridinoline (they are degradation products of collagen cross–links), peptide fragments of collagen with deoxypyridinoline couplings belong to pyridinium compounds).
Carboxy-terminal telopeptides of collagen are formed by degradation of mature collagen fibers.
_
Selected bone diseases
Osteoporosis
Osteoporosis is systemic bone disease characterized by low bone density and altered bone microarchitecture with consequent increase in fragility. Its substrate is the loss of inorganic and organic bone matter which leads to increased fracture risk. Osteoporosis is divided into two types – primary osteoporosis (cause is unknown, e.g. postmenopausal or senile osteoporosis) and secondary osteoporosis (cause is known, e.g. endocrine problems, medicaments, immobilization). Osteoporosis is a serious health problem – it affects 7-8 % of the population in the Czech republic and approximately 1/3 of menopausal women.
Osteomalacia (in an adulthood) / rickets (in a childhood)
These diseases are caused by an inadequate or delayed mineralization of osteoid. It is predominantly the loss of inorganic bone matter (bone decalcification), resulting in a softening of bones and their deformities (typical deformity of skull, spine, chest and long bones in rickets).
A lack of vitamin D (calcitriol is an active form of vitamin D, its importance in the bone metabolism is mentioned above) is the most common cause of osteomalacia. Its deficiency leads to hypocalcemia, in which the body reacts by increased secretion of parathormone. This hormone among others, changes the ratio Ca2+ / phosphates (↑ calcemia and ↓ phosphatemia). Resulting disproportion does not allow to store mineral matter in osteoid. Vitamin D deficiency can be caused by the inadequate intake or kidney disease.
Subchapter Authors: Josef Fontana and Petra Lavríková