Content:
1. Coronary artery disease (CAD)
2. Valve disease
3. Heart failure
4. Arrhythmia
5. Ion disbalance
6. Hypertension
7. Edema
_
Coronary artery disease (CAD)
During physical exertion the heart muscle consumes more oxygen. It’s delivery is provided by increased blood flow in coronary arteries and it can be increased up to 5 fold. This mechanism is called coronary flow reserve. Thus the oxygen consumption is one of the basic factors affecting coronary blood flow. In case that there is atherosclerotic plaque in coronary artery, the patient may experience symptoms of hypoperfusion of the heart muscle. These plaques can narrow the coronary arteries and can cause symptoms such as chest pain (angina pectoris) or shortness of breath. Complete occlusion of coronary artery can cause myocardial infarction. This is reflected as an acute ST segment elevation on the ECG (in longer term there can be a pathological Q wave), followed by loss of ability to contract and chest pain mediated by autonomous nerve system. From histopathological point of view there is a necrosis of cardiomyocytes, starting from subendocardium to subepicardium. Extent of necrosis depends on the size of the area that is supplied by an enclosed artery, and also depends on the duration of the closure. The only way of solution (getting blood delivery to the area of hypoperfusion) is to restore perfusion in closed artery by percutaneous coronary intervention (PCI) or by cardiac surgery (coronary artery bypass graft). In past the thrombolysis was used as well, but in these days PCI and cardiac surgery are the method of choice. Myocardial infarction can be complicated by arrhythmias, heart failure or by mechanical complications such as rupture of the heart wall, ventricular septum or papillary muscle.
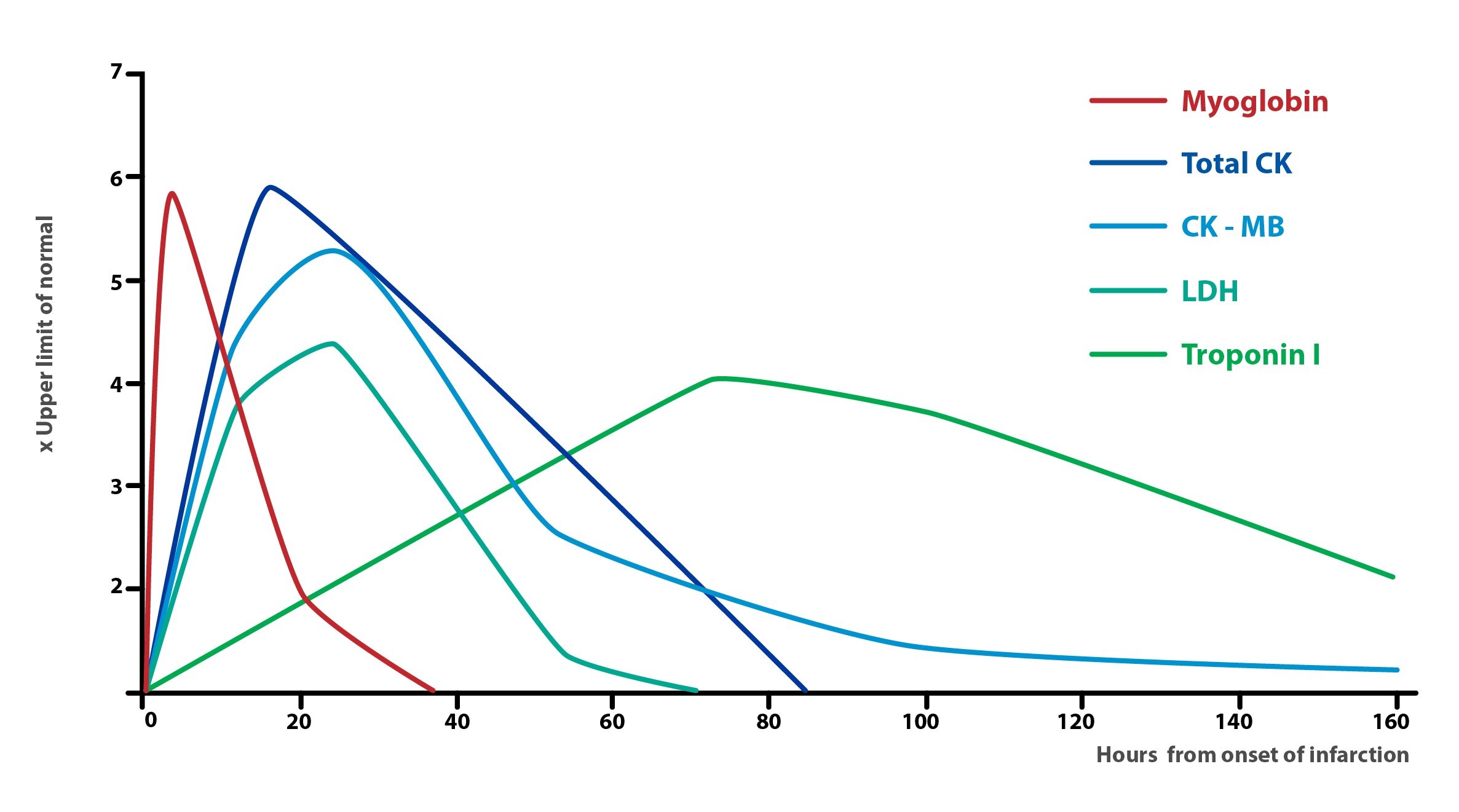
During the cardiomyocytes’ damage the intracellular substances such as troponin T, I (different from the troponin in skeletal muscles) are released into the blood and can be tested as a marker of cardiomyocytes’ necrosis. The other substances such as creatine kinase (CK) and its isoenzyme CK-MB, myoglobin and AST, which are not so specific as troponin, are also released into to the blood.
_
Valve disease
Valve disease is caused by valvular insufficiency or valvular stenosis. Valvular insufficiency leads to the backflow (regurgitation) of the blood (into the atrium or ventricle) and causes volume overload. Valvular stenosis leads to increased pressure and decreased blood flow when the blood has to be pushed through stenotic area, it causes pressure overload. Untreated valve disease leads to heart failure.
_
Heart failure
Heart failure is a condition when the heart muscle is not able to pump the needed amount of blood to ensure metabolic demands of the body’s tissues or does it with plugged compensating mechanisms. Heart failure can be caused by many conditions, diseases such as coronary artery disease, hypertension, valve disease, cardiomyopathies, myocarditis, etc. Acute heart failure can be caused by acute myocardial infarction, arrhythmia etc. Chronic heart failure develops slowly for example due to valvular disease.
Another possible division is the division of the systolic heart failure, which occurs for example during volume overload, myocardial disease (decreased contractility) or pressure overload, and diastolic heart failure caused by increased rigidity of the chamber wall.
As markers for heart failure are currently used in practice natriuretic peptides – BNP (NT-proBNP).
_
Arrhythmia
All cardiomyocytes are endowed with the ability to create action potential – cardiac automaticity. Physiologically the action potential is generated only in pacemaker cells. These cells spontaneously depolarize during diastole and after reaching the threshold the membrane depolarization (action potential) is triggered. Various parts of heart’s electrical conduction system have different frequency of spontaneous depolarization. Sinoatrial node and atrioventricular node have slow speed of propagation of the action potential, but they have quite high frequency of spontaneous depolarization. In some pathological situations, such as hypoxia, ion imbalance (mainly K+ and Ca2+), excessive stimulation of adrenergic receptors, lowering of the temperature or the effect of some drugs, can the other cardiomyocytes be a source of depolarization (action potential) and thus myocardial contraction.
The heart beats with normal sinus rhythm in the range of 60-90 beats per minute. Physiologically, the heart rate slows down during sleep (bradycardia) and it accelerates for example during exercise (tachycardia). In young people the sinus arrhythmia may occur during respiration. The tonic activity of vagus nerve is inhibited in deep inspiration and thus the frequency increases, in opposite during expiration the frequency of the heart decreases. Under certain conditions the sinus bradycardia and sinus tachycardia are pathological. Then there are arrhythmias. Supraventricular arrhythmias like for example atrial fibrillation (AF), which is most common. Disorganized electrical impulses in AF originating in the roots of the pulmonary veins and other places of atrium with irregular conduction to ventricles. Another example of supraventricular arrhythmia is atrial flutter with regular conduction to ventricles caused by reentry loop.
In case of pacing the heart rhythm from ventricular conduction system, the rate slows down to 30-40/min and QRS complexes on the ECG are wider than 120 ms. In ventricular fibrillation the depolarization of cardiomyocytes is caused by several mechanisms – reentry, triggered activity, ectopic foci of excitation or combination of these. In ventricular fibrillation (VF) the heart work is ineffective, fibrillating ventricals are not pumping blood and the circulation stops. As an effective therapy of VF there comes a defibrillation. Ventricular extrasystole is a contraction that arises from ectopic foci in the area of Purkinje fibers, it has wide QRS complex. Supraventricular extrasystole is characterized by slender QRS complex.
Arrhythmias can also occur if there is a problem in the conduction system of the heart. In case of interruption of the conduction between the atria and the ventricles (the complete atrioventricular block), the ventricular pace rhythm is activated (30-40/min). If the conduction is interrupted in the area above the AV node, AV node or the conduction part of nodal junction becomes the pacemaker with a frequency of 50/min. This is called junctional rhythm. If there is a problem with conduction from the atria to the ventricles (slow conduction, partial block, etc.), it leads to incomplete atrioventricular block. If the conduction is interrupted behind the His bundle, it creates the bundle branch block (complete or partial, left block, right block or bifascicular block).
_
Ion disbalance
The activity of the heart is affected by the level of ions in blood and in intracellular compartment. The most important ions for the heart function are K+, Ca2+ and Na+.
Potassium
K+ takes the task of maintaining the membrane potential, which in disorder of K+ homeostasis becomes more negative (in hypokalemia ) or less negative (in hyperkalemia) . This affects the excitability of electrically active tissues. K+ intake is not significantly regulated. After uptake of large amount of K+ is the most of it is under the influence of insulin moved from the blood into the cells (about 80 %), from where it is slowly released and eliminated by the kidneys.
The transfer of K+ into cells is influenced by various factors:
1 ) Increased EC concentration of K+ increases the activity of the Na+/K+-pump
2 ) Insulin energizes Na+/K+-pump
3) Epinephrine – through β2-receptors stimulates Na+/K+-ATPase (α2-receptors inhibit Na+/K+-pump)
4 ) Aldosterone increases the transfer of K+ into the cells, but in the kidney aldosterone causes increased urinary excretion of K+
5 ) pH – in alkalosis when the extracellular fluid has lack of protons, H+ emerges from the cells in the exchange for K+ (if positive ion exits from the cell, then it must be replaced by another positive ion). In acidosis opposite action happens, when the pH is compensated by transferring H+ into the cells, ions of K+ are in exchange released.
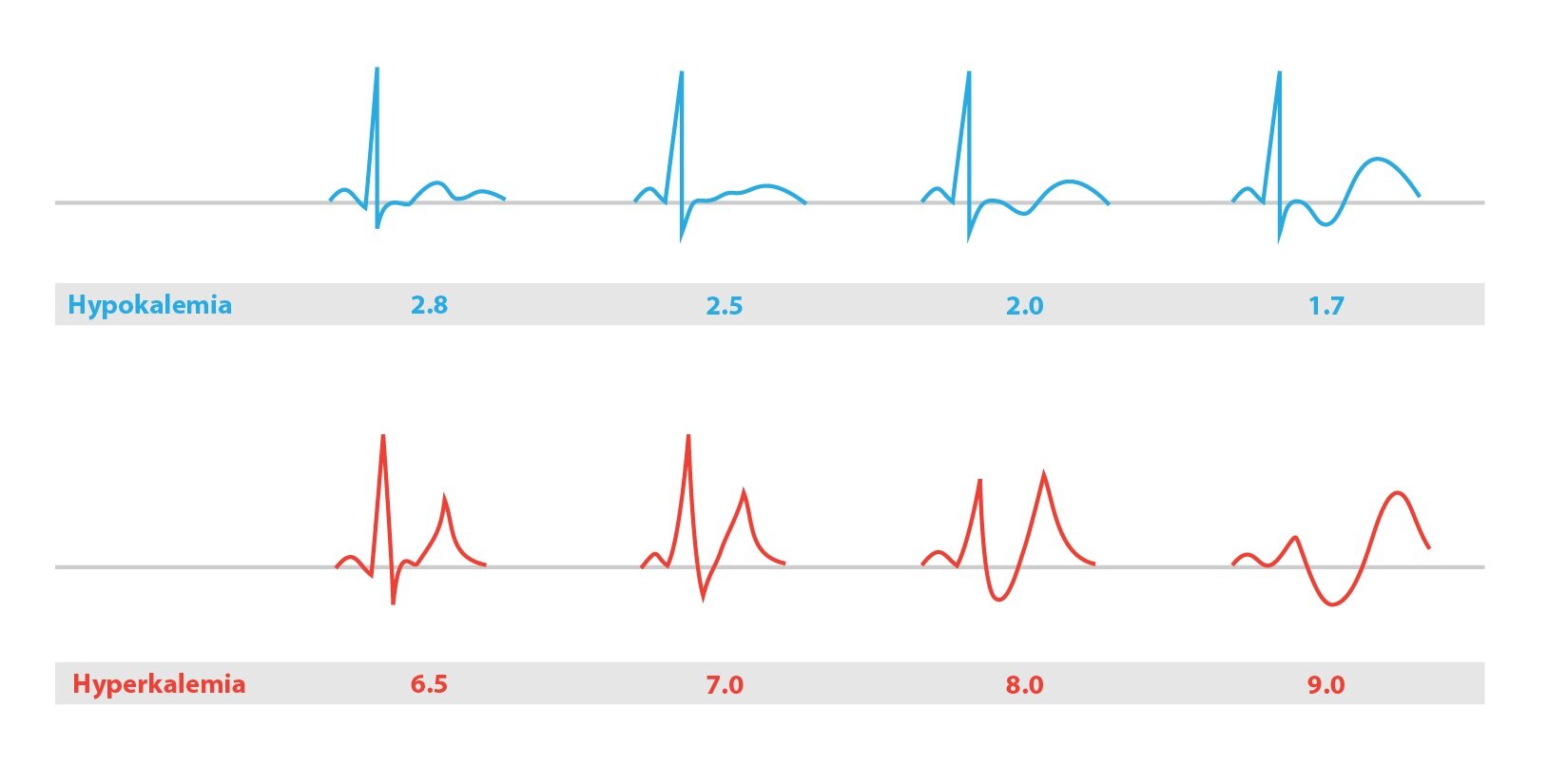
In hyperkalemia the membrane potential becomes less negative, therefore in first phase of hyperkalemia it is easier to induce stimuli. The excitability is increased, arrhythmias can occur, patients have paresthesias. In severe hyperkalemia is the membrane potential even less negative, sodium channels stay inactive and second phase of hyperkalemia comes with with muscle weakness, paralysis, bradycardia and QRS widening on ECG. In case of extreme hyperkalemia the whole process can end with ventricular fibrillation or the heart stops in diastole (asystole).
Hypokalemia occurs when the total body amount of K+ is decreased, rarely it is caused by bigger transfer of K+ into the cells. Symptoms and signs become evident when the level of K+ is lower than 3 mmol/l. Real deficit of K+ is caused by it’s inadequate intake (starving, anorexia, alcoholism), profuse sweating, diarrhea, vomiting (direct loss of K+, indirect loss because of alkalosis and because of increased secretion of aldosterone caused by water loss) or it’s increased renal excretion (diuretics, hyperaldosteronism, hypercorticism, polyuric phase of kidney failure). Relative K+ deficiency is caused by it’s increased move to cells in acute alkalosis or sudden massive increase in circulating insulin. In hypokalemia the conduction of action potential in heart is prolonged, extrasystoly occur. On ECG the T waves get flatten, U wave can occur. Severe hypokalemia can cause ventricular arrhythmia including ventricular fibrillation.
Calcium
For myocardium and for neuromuscular excitability is mainly important the ionized fraction of calcium. It’s decrease results in higher excitability, it’s increase in contrast stabilizes the membranes and reduces the excitability of cells. The increase of intracellular concentration increases the excitability of the cells (e.g. during tissue hypoxia). Calcium ions are responsible for the contraction of the heart, but at the same time the cardiomyocytes has not sufficiently developed sarcoplasmic reticulum, thus a heartbeat, is significantly dependent on extracellular calcium.
When Ca2+ levels are higher than 4 mmol/l a hypercalcemic crisis appears – confusion, unconsciousness and cardiac arrest in systole. Hypercalcemia shortens the action potential, which is reflected in the ECG with QT interval shortening. Severe hypercalcemia leads to a reduction of the amplitude of T waves and may also cause their inversion. In hypocalcemia QT interval is prolonged and can lead to triggering ventricular arrhythmia.
_
Hypertension
Blood pressure is determined by cardiac output and by peripheral vascular resistance. Optimal blood pressure in relationship to cardiovascular risk is 120/80 mmHg. Hypertension is defined by blood pressure 140/90 mmHg and higher. For the diagnosis of hypertension we need to measure these values at least two times from three, in two separate visits at the doctor.
Untreated hypertension leads to pressure overload of left ventricle. In first time there is a compensatory hypertrophy of the ventricle, but from the long term of view it leads to heart failure and other organ damage. We distinguish two types of hypertension. First one is primary (essential) hypertension, second one is secondary hypertension.
The primary (essential) hypertension affects about 95 % of patients with hypertension. It is a multifactorial disease and we still today don’t know all of the factors which are involved.
Secondary hypertension is caused by detectable organic cause, for example some endocrinological disorders (primary hyperaldosteronism, pheochromocytoma, or Cushing’s), renal cause – renovascular hypertension, sleep apnoea syndrome, aortic coarctation, etc. Secondary hypertension affects about remaining 5 % of patients.
_
Edema
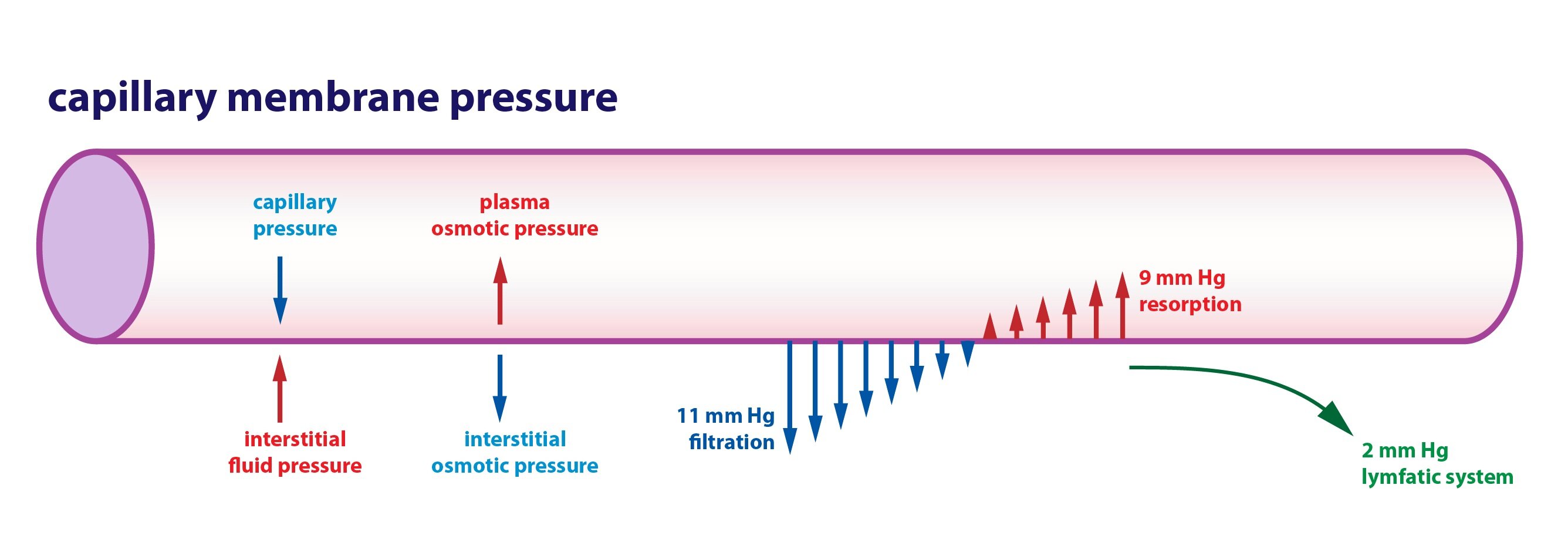
Edema is an accumulation of fluid in the interstitium in abnormal amount. Changes in the amount of fluid in the interstitium can have several general causes: increased hydrostatic pressure in the capillary, decreased plasma proteins (albumin), osmotically active substances in the interstitium, increased capillary permeability, or failure of lymphatic drainage.
Subchapter Authors: Peter Ivák, Josef Kroupa, Patrik Maďa and Josef Fontana