Content:
1. Functional morphology of the respiratory system
_
Functional morphology of the respiratory system
Functionally, the respiratory system is divided into conducting portion and respiratory portion (in lung alveoli is present a barrier to gas exchange between the atmosphere and the blood). Conducting portion is divided into upper respiratory tract (nasal cavity, paranasal sinuses and nasopharynx) and lower respiratory tract (larynx, trachea, bronchi, bronchioles). Respiratory part is represented by respiratory bronchioles and alveoli.
Conducting portion
Nasal cavity
Mucosa of nasal cavity warms and moistens the inspired air containing tiny particles which are trapped in the mucosal layer (filtration of inspired air). Nasal cavity is divided into external nasal vestibule and proper nasal cavity. Nasal vestibule is lined by nonkeratinized stratified squamous epithelium with transition to ciliated pseudostratified columnar epithelium. Nasal vestibule also contains short thick hair. Proper nasal cavity is divided by cartilaginous and bony septum into two cavities. In each cavity are found the nasal conchae (conchae nasales superiores, mediae et inferiores). Inferior and medial conchae are covered by ciliated pseudostratified columnar epithelium. The superior conchae are covered by pseudostratified columnar epithelium with olfactory receptor cells. Whole nasal cavity is highly vascularized.
Nasopharynx (pars nasalis pharyngis)
Nasopharynx is lined by ciliated pseudostratified columnar epithelium. The lymphatic tissue is organized into tonsils.
Larynx
Larynx is lined by ciliated pseudostratified columnar epithelium except vocal cords (lined by stratified squamous epithelium). The wall of larynx is reinforced by cartilage tissue. Large cartilages (cartilago thyroidea, cartilago cricoidea) and part of cartilago arytenoidea are composed of hyaline cartilage. Small cartilages (cartilagines corniculatae, cuneiformes et arytenoides) are composed of elastic cartilage tissue. Laryngeal inlet is protected by epiglottis consisting of elastic cartilage. Epiglottis is covered by nonkeratinized stratified squamous epithelium with transition to ciliated pseudostratified columnar.
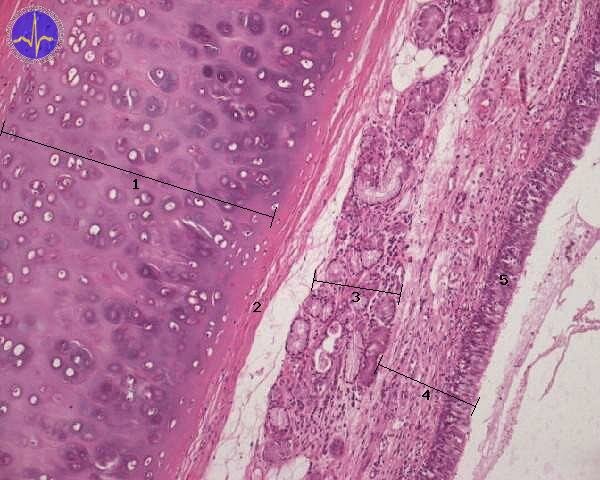
Trachea
Trachea is air tube about 12 cm long lined by ciliated pseudostratified columnar epithelium. Submucosa contains seromucous glands and 16 to 20 C-shape hyaline cartilages.
1 – Hyalinne cartilage, 2 – Perichondrium, 3 – Seromucinous glands, 4 – Tunica mucosa, 5 – Pseudostratified columnar epithelium with cilia
Lungs (pulmones)
Lungs are paired organs. Four developmental phases of lungs are distinguished:
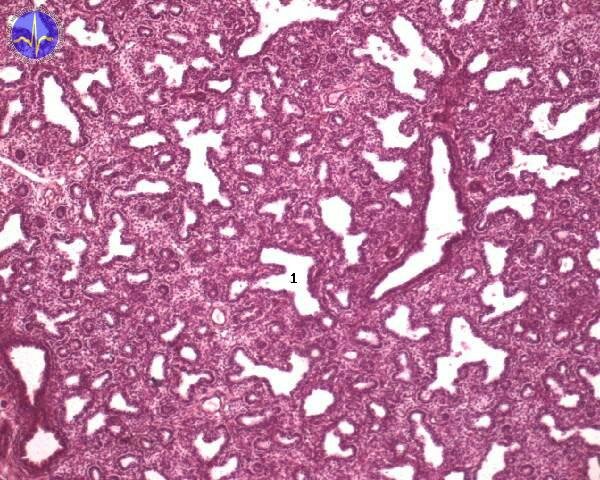
1) Pseudoglandular phase (5.-17. week) Lung tissue resemble endocrine gland, bronchi and bronchioles are formed. Respiration is not possible yet.
2) Canalicular phase (8.-24. week) The respiratory bronchioles and alveolar ducts are formed.
Fetal lungs in canalicular phase
3) Saccular phase (25.-36. week) The epithelial cells differentiate and the production of surfactant initiates.
4) Alveolar phase (37. week – 8. year) The alveoli are developed.
The right lung is composed of 3 lobes, the left one of 2 lobes. Trachea divides in bifurcation into two main bronchi entering the lung in the hilum. Main bronchi (primary bronchi) divide into lobar bronchi (secondary bronchi) – three on the right side and two on the left side. Lobar bronchi branch into tercial segmental bronchi – 10 on the right side and 8 on the left side.Terminal bronchioles branch into 2 or more respiratory bronchioles and they branch again into alveolar ducts (2 to11 branches). At the blind-ending alveolar ducts occur alveolar sacs and alveoli. During the branching of bronchial tree, structure of the wall of air tubes changes – cartilage tissue disappears and the amount of smooth muscle cells and elastic fibers decreases. Large bronchi are lined by ciliated pseudostratified columnar epithelium and their loose connective tissue contains lymphatic follicles and immune cells – lymphocytes, macrophages, plasma cells producing immunoglobulins A and seromucous glands.
Small bronchioli are also lined by ciliated pseudostratified columnar epithelium but they contain less goblet cells.
Bronchioles with smaller diameter than 1 mm are lined by the same epithelium, but their wall lacks cartilage and glands. Numerous smooth muscle cells and reticular fibers are found here. Bronchioles branch into terminal bronchioles lined by simple columnar epithelium containing nejsou to pohárkové bb! Clara cells. These cells produce specific proteins responsible for defence of mucosa. Terminal bronchioles branch into respiratory bronchioles lined by simple ciliated columnar or cuboidal cells and Clara cells. Respiratory bronchioles then branch into alveolar ducts, alveolar sacs and alveoli.
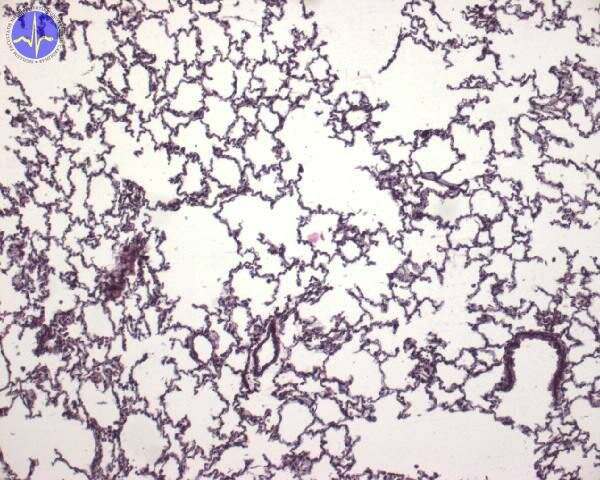
Pulmonary tissue
Alveoli
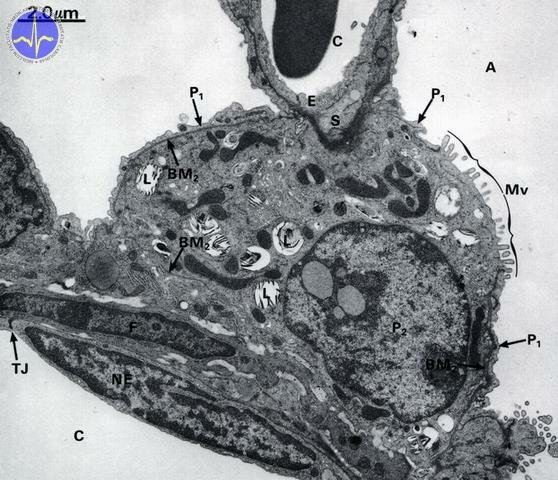
The alveolar lining composed of pneumocytes. Pneumocytes are distinguished into type I (also called membranous) and type II (also called granular) pneumocytes.
1) Type I pneumocytes – are flattened cells covering about 97 % of alveolar surface lining but they represent only 40% of total cellular count in alveoli.
2) Type II pneumocytes – they exhibit secretory characteristics and are responsible for production of surfactant. Their cytoplasm contains lamellar bodies with surfactant.
Electron micrograph of a flattened type I pneumocyte (P1) and large type II pneumocyte producing surfactant (P2)
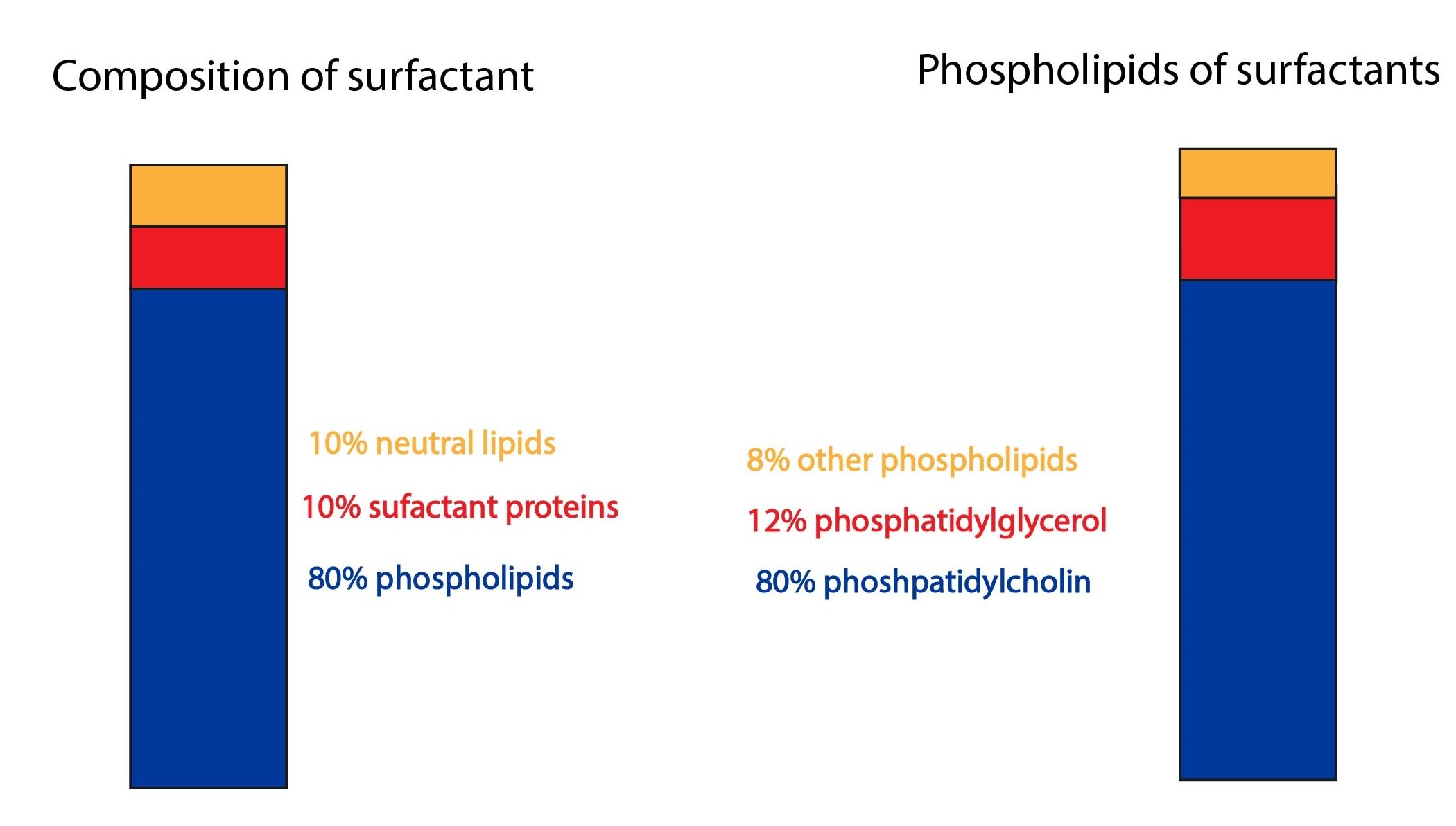
Surfactant is protein-rich fluid with superficial layer of phospholipids. Production begins in 24th week of fetal development. Surfactant decreases the alveolar surface tension on the air-blood barrier and thus, the power required for expansion of lungs decreases. It also prevents the collapse of alveoli. Production and maturity of surfactant is important for survival of premature infants. Production of surfactant can be increased by intramuscular application of cortisol to mother with threatened premature delivery.
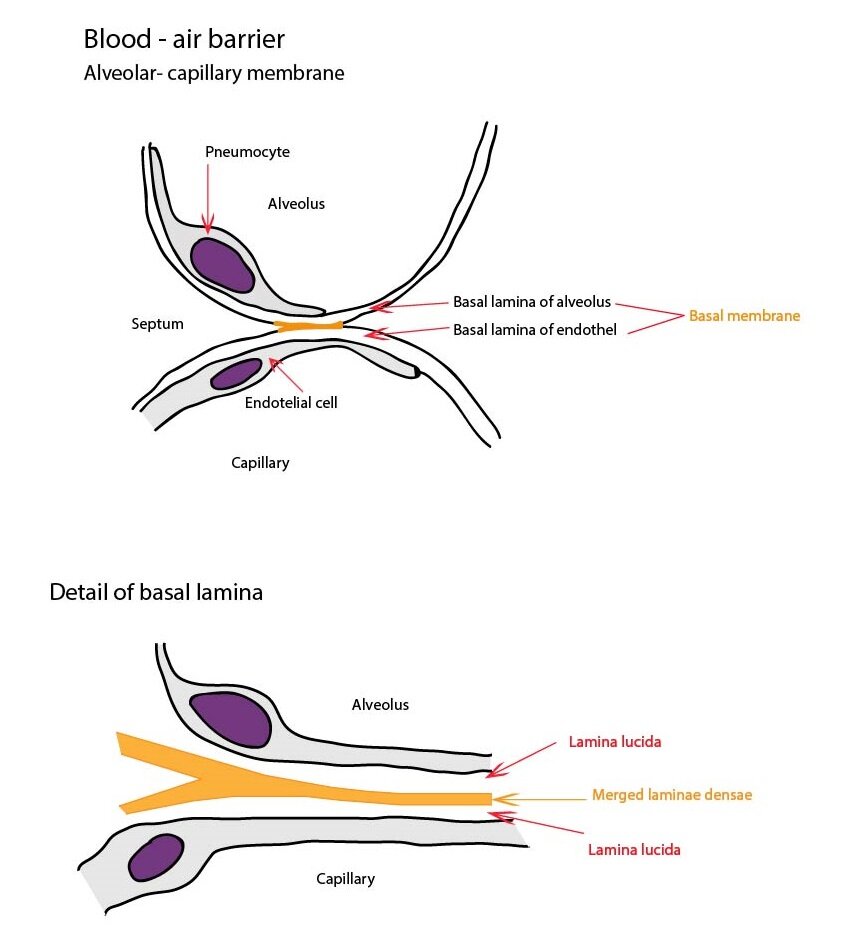
Air-blood barrier
Air-blood barrier is composed of type I pneumocyte, basal membrane and endothelial cell lining the capillary. Functionally, it is the most important structure in the alveolar septum. This barrier enables the gas exchange. The oxygen molecules diffuse from alveoli to the blood and carbon dioxide in the opposite direction.
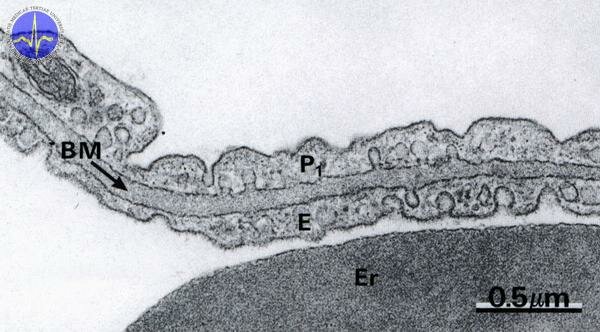
Electron micrograph of air-blood barrier composed of basal membrane (BM), type I pneumocyte (P1) and endothelial cell (E). The large dark structure in the inferior part of micrograph is erythrocyte in capillary.
The lung circulatory system is distinguished into nutritive and functional. The functional circulatory system is represented by pulmonary arteries and veins. The nutritive system is created by bronchial arteries.
Pleura
Pleura consists of two serous membranes – parietal and visceral. Both membranes are formed by connective tissue layer containing collagenous and elastic fibers. This layer is covered by mesothelium. Between visceral and parietal membranes, the pleural cavity occurs. Pleural cavity contains small amount of fluid which facilitates movements during respiration.
Subchapter Authors: Martina Šajdíková and Lucie Nováková