Content:
1. General organization of the gastrointestinal tract
2. Morphology of individual digestive organs
_
General organization of the gastrointestinal tract
The wall of gastrointestinal tract, especially the portion that extends from the esophagus to the anal canal, has the same basic structural organization. It’s formed by 4 distinctive layers from the lumen outward, they are as follows:
1) Mucosa (tunica mucosa)
2) Submucosa (tunica submucosa)
3) Muscular coat (tunica muscularis)
4) Serosa (tunica serosa) or adventitia (tunica adventitia)
1) Tunica mucosa (mucosa)
Tunica mucosa lines the internal surface of the alimentary canal. It has three principal functions: protection of the inner environment, secretion and absorption. Typical mucosa consists of three layers: a lining epithelium (lamina epithelialis), lamina propria mucosae and lamina muscularis mucosae.
Epithelium
The mucosal surface is covered by epithelial layer, which is in direct contact with a content of alimentary canal. Type of the epithelium differs throughout the alimentary canal and is adapted to the specific function of each part of the tube. In the oral cavity, esophagus and anal canal is protective nonkeratinized stratified squamous epithelium. The rest of tube is lined by simple columnar epithelium.This simple columnar epithelium has also the secretory function, especially in stomach, and resorptive function in intestines. In the mucosa of some parts of alimentary canal are dispersed cells with endocrine secretory function (enteroendocrine cells). These cells more numerous in lower part of stomach and proximal part of small intestine.
Lamina propria mucosae
This loose collagenous connective tissue layer is covered by mucosal epithelium. It contains a lot of blood and lymphatic vessels and accumulation of lymphocytes represented by diffuse lymphatic tissue or lymphatic follicles. The lamina propria contains mucosal glands throughout the length of alimentary canal. In some parts the glands extend through the entire width of lamina propria (e.g. in stomach). The lamina propria mechanically supports the epithelium and binds it to the third layer (muscularis mucosae).
Lamina muscularis mucosae
The muscularis mucosae is a layer of smooth muscle tissue localized between mucosa and submucosa. It’s contraction produces movement of the mucosa independent of the peristaltic movement of entire wall of digestive tract.
2) Tunica submucosa (submucosa)
The submucosa consists of a loose collagenous connective tissue. This layer is highly vascularized and contains submucosal nerve plexus – plexus submucosus Meissneri, part of autonomic enteric nervous system primarily responsible for control of glandular secretion. In several parts of alimentary canal contains submucosa also glands (e.g. in esophagus or duodenum).
3) Tunica muscularis (muscular coat)
Tunica muscularis externa consists of two layers of smooth muscle (in upper one third of esophagus is also striated muscle) organized into inner circular and outer longitudinal layer. Between these two muscle layers is a thin connective tissue layer containing blood and lymphatic vessels and myenteric nerve plexus – plexus myentericus Auerbachi, which is responsible for motility. Both of mentioned plexus have the same number of neurons as a spinal cord. The circular smooth muscle layer forms sphincters at specific locations along the digestive tract – pharyngoesophageal sphincter, pyloric sphincter, ileocecal valve and internal anal sphincter.
4) Tunica serosa
The serosa covers organs in the peritoneal cavity. It consists of one layer of simple squamous epithelium – the mesothelium, and an underlying connective tissue layer. The adventitia consists of connective tissue which covers organs situated outside the peritoneal cavity. It does not contain mesothelium. It is found in parts of alimentary canal directly attached to surrounding structures.
The resorption in the digestive tract is possible because of projections of the mucosa and submucosa into the lumen. These structures greatly increase the surface area available for resorption. The following structural specializations can be distinguished:
1) Plicae circulares
Plicae circulares are submucosal folds oriented perpendicularly to the long axis. They are present along most of the length of the small intestine, they decrease towards ileum.
2) Villi intestinales
Villi are mucosal projections covering entire surface of the small intestine, they are the principal site of resorption of the products of digestion.
3) Microvilli
Microvilli are microscopic projections of the apical surface of intestinal absorptive cells.
The secretory function of mucosa provides the lubrication of the epithelial surface and produces enzymes, hormones and antibodies into the lumen of alimentary canal. The glands associated with the digestive tract develop from invaginations of the luminal epithelium and include:
1) Mucosal glands that extend into the lamina propria
2) Submucosal glands that deliver their secretions directly to the lumen of mucosal glands or via ducts that pass through the mucosa to the luminal surface
3) Extramural glands (liver, pancreas) lie outside the digestive tract and deliver their secretions via ducts to the lumen of alimentary canal.
_
Morphology of individual digestive organs
Oral cavity
The both spaces of oral cavity (vestibule and oral cavity proper) are lined by the oral mucosa that consists of stratified squamous epithelium. The underlying connective tissue lamina propria creates deep penetrations of the connective tissue papillae into the epithelium and isn’t well distinguished from submucosa. The submucosa contains minor salivary glands. in the area of hard palate is no submucosal layer.
Lip
The outer surface of the lip is covered by thin skin, inner surface by the oral mucosa – the transitional zone is the free edge (or vermillion border). The outer cutaneous part is covered by keratinized stratified squamous epithelium with skin appendages (hair follicles, sebaceous glands, sweat glands).
The vermillion is covered by thick nonkeratinized stratified squamous epithelium which lacks sweat glands and hair follicles, sebaceous glands are here present independently. Inner side of the lip is lined by oral mucosa consisting of nonkeratinized stratified squamous epithelium. Papillae of the lamina propria are irregular. The submucosal layer contains mucous minor salivary glands. Mucosa is anchored to the orbicularis oris muscle by stripes of dense connective tissue.
Cheek
The cheek resembles the inner side of lip in histologic features.
Hard palate (palatum durum)
The mucosa consists of parakeratinized stratified squamous epithelium. Lamina propria mucosae is attached directly to the periosteum of bony palate, which makes the mucosa immobile. This connection of mucosa and periosteum is called the mucoperiosteum. This area lacks the submucosa.
Soft palate (palatum molle)
The soft palate is located at the back of the roof of mouth and is connected to the hard palate.
The mucosa of the oral side is covered by nonkeratinized stratified squamous epithelium. Under the mucosa are short and wide connective tissue papillae. Lamina propria mucosae contains collagenous and elastic fibers. Submucosa is well defined and contains numerous mucous minor salivary glands. Submucosa adheres to the striated muscle of the soft palate.
The mucosa of the nasal side of soft palate is lined by ciliated pseudostratified columnar epithelium with goblet cells. Under the epithelium is connective tissue layer containing seromucous tubuloalveolar glands.
Tongue
The tongue is muscular organ covered by mucosa, located on the inferior surface of the oral cavity. The lingual mucosa differs on the dorsal and inferior surface.
Mucosa on the inferior side of the tongue is not special, it is relatively thin, covered by nonkeratinized stratified squamous epithelium. The papillae of lamina propria are short and numerous. Submucosa is formed by loose collagenous connective tissue and surrounds underlying muscle bundles. The thin epithelium and highly vascularized mucosa of inferior lingual side permit sublingual application and rapid absorption of some drugs.
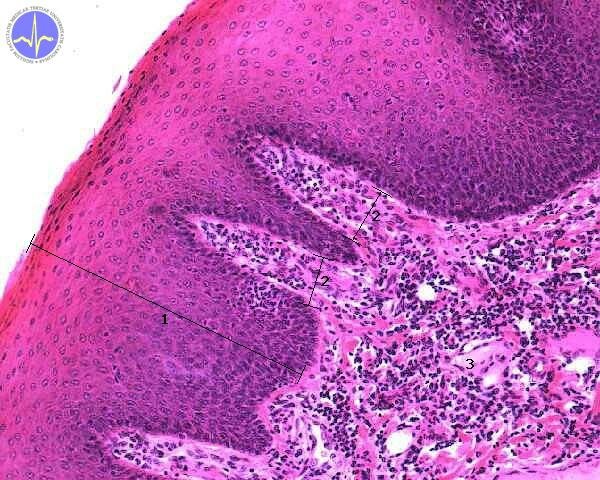
1 – Stratifeid squamous epithelium, 2 – Papila in lamina propria, 3 – Lamina propria
Dorsal surface of the tongue is covered by specialized mucosa. Sulcus terminalis (V-shaped groove) divides the tongue into an anterior two thirds (oral part) and a posterior one third (pharyngeal part, root of the tongue). These two parts differ in embryonal origin and due to that also in innervation.
The mucosa of dorsal surface of the tongue is covered by lingual papillae (papillae linguales) which create its characteristic appearance. Each papilla is composed by elongated projections of connective tissue that are covered by keratinized (or nonkeratinized – it depends on the type of papilla) stratified squamous epithelium. The dorsal lingual surface lacks the submucosal layer.
According to shape and structure, four types of papillae are describe:
1) Papillae filiformes (filiform)
2) Papillae fungiformes (fungiform)
3) Papillae foliatae (foliate)
4) Papillae circumvallatae (vallate)
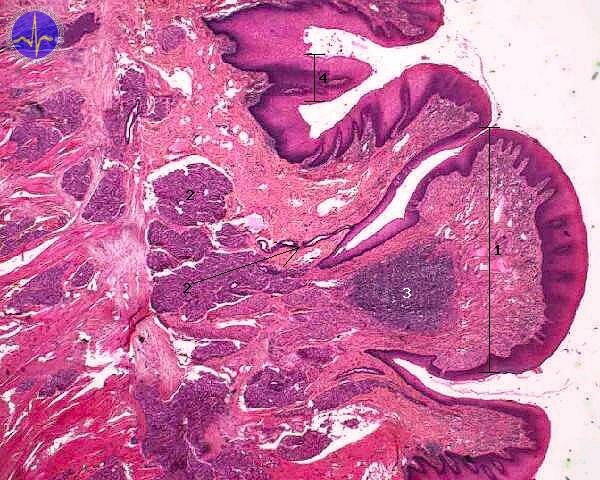
1 – Circumvallate papilla, 2 – Ebner’s gland + duct (arrow), 3 – Lymphatic follicle, 4 – Filliform papilla
Mucosa of the anterior two thirds of lingual surface is frequently covered by keratinized filiform papillae. Apices of filiform papillae are highly keratinized. (keratinized caps).
Fungiform papillae are bigger and less numerous than filiform papillae. They are dispersed between filiform papillae. The covering epithelium is thin nonkeratinized and contains taste buds.
Foliate papillae occur on the posterior parts of the lateral edges of the tongue. They are arranged in 1 or 2 lines. Covering epithelium is nonkeratinized, in some places containing taste buds.
Circumvallate papillae are arranged anterior to the sulcus terminalis into the V-shape line. The apex of this line is located in foramen caecum (the remnant of the site from which an envagination of the endoderm occured to form the thyroid gland – ductus thyreoglossus). Human tongue has 8 to 12 these papillae, they are the largest papillae. Covering epithelium is nonkeratinized and on the lateral sides contains numerous taste buds. Ducts of serous von Ebner’s glands empty into the moats around the papillae. Near the papillae on the dorsal lingual surface are also mucous Weber’s glands.
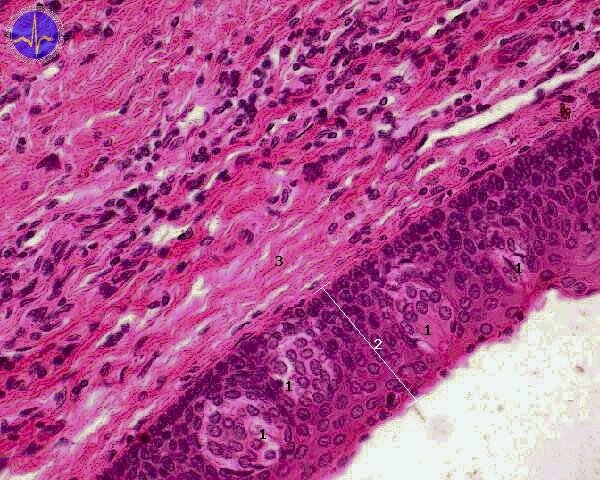
1 – Taste bud, 2 – Epithelium, 3 – Lamina propria
Salivary glands
Salivary glands are exocrine glands. Their primary function is secretion of saliva. The major salivary glands compose of two principal components – secretory epithelium and supporting connective tissue stroma. Macroscopically, major salivary glands are formed by secretory acini organized into lobules. The branching of the duct system is described as follows:
main excretory duct branches into the interlobular ducts. This repetitive branching is dichotomic. Terminal branches enter into the lobuli as intralobular ducts. In the lobuli continues the branching and gives rise to the striated ducts, then intercalated ducts and final secretory acini. Secretory units are serous, mucous or mixed. The relative frequencies of three types of secretory units are a prime characteristic by which the major salivary glands can be distinguished.
Intercalated duct is lined by simple cuboidal epithelium, striated duct is lined by simple columnar epithelium. Cells of striated duct possess numerous infoldings of basal plasma membrane. Their nucleus typically occupies the upper portion of cell. Intercalated and striated ducts actively modify the composition of secretion. In some glands (especially in parotid gland) is significant adipose tissue.
Serous cell has a pyramidal shape with apex facing the lumen. Basal portion of the cell contains nucleus and numerous rough endoplasmic reticulum which causes basophilia of cells. Apical portion of cell is filled with eosinophilic zymogen granules. Serous cells produce watery fluid with high content of proteins.
Mucous cells have columnar shape and flattened nucleus contained in the basal portion. Cell is filled with mucinogen granules which are dissolved during histological staining and therefore, these cells usually appear pale or empty. Secretion is viscous and mucous.
Both serous and mucous cells can be arranged into bulbous structures called acini. localized at the endings of mucous tubuli.
Major salivary glands involve:
1) Glandula parotis (Parotid gland)
The largest salivary gland is completely serous with tubuloacinar structure. The duct system consists of long branching intercalated ducts. Striated ducts are prominent. Parotid gland contains large amount of adipose tissue which distinguishes it from also serous pancreas. .
2) Glandula submandibularis (Submandibular gland)
Submandibular gland is mixed gland mostly serous in humans. Intercalated ducts are shorter and striated ducts are long and prominent.
3) Glandula sublingualis (Sublingual gland)
Sublingual gland is mixed gland mostly mucous in humans. Mucous cells stained with hematoxylin-eosin are pale. Duct system is less developed. Striated ducts are short and less prominent.
Teeth
Children have 20 deciduous (primary) teeth. First tooth to erupt (usually in the mandible) is incisor tooth at approximately 6 months of age. But in some infants the first tooth may not occur until 12-13 months of age. During the life (usually between 6 and 13 years of age) deciduous teeth are replaced by permanent teeth. In adult 32 permanent teeth are found. Each quadrant consist of 8 teeth (2 incisors, 1 canine tooth, 2 premolar teeth and 3 molar teeth).
Teeth consist of several layers of specialized tissues:
1) Enamel
2) Dentin
3) Cementum
Tooth is composed of several parts – crown and one or more roots. Each tooth is embedded in the alveolar process. Crown is covered by enamel and root by cementum. These layers encounter in cementoenamel junction at neck (cervix). Tooth is filled with dentin containing the pulp chamber. Periodontal collagen fibers attach the tooth into the alveolus.
Enamel
Enamel is the hardest substance in the human body, it consist of 96 % calcium hydroxyapatite. It is acellular mineralized tissue covering the crown of tooth. Enamel is produced by ameloblasts derived from ectoderm.
Dentin
It is calcified material produced by odontoblasts. It forms most of the tooth. odontoblasts line the inner surface of tooth and separate it from pulp chamber. Odontoblasts are derived from neural crest.
Cementum
Cementum covers the root of tooth. It is avascular tissue.
In the text below are shortly described the differences in structure of individual parts of digestive tract and how they differ from general organization of alimentary canal described in the beginning.
Esophagus
Esophagus is a muscular tube connecting pharynx and stomach. It consists of four typical layers and lumen has branched appearance due to numerous longitudinal foldings.
Tunica mucosa
Tunica mucosa is lined by nonkeratinized stratified squamous epithelium. The borderline between epithelium and lamina propria is not distinct and numerous papillae extend toward the basal portion of epithelium. In the connective tissue core of the papillae are blood vessels and nerves. lamina propria contains numerous lymph follicles (mucosa-associated lymphoid tissue, MALT) especially around gastroesophageal junction. Also small tubular mucous glands are found here. Lamina muscularis mucosae is composed of mostly longitudinal smooth muscle.
Tunica submucosa
It consists of fibroelastic connective tissue with numerous blood and lymphatic vessels and mucous glands (glandulae oesophageales). Esophageal glands are small tuboalveolar glands localized in lamina propria and submucosa which empty into the lumen via long ducts. They are almost completely mucous. In the area of gastroesophageal junction are gland predominantly in lamina propria mucosae (esophageal cardiac glands) and they resemble gll. cardiacae of stomach.
Tunica muscularis
Tunica muscularis composes of outer longitudinal and inner circular layer. Upper third of esophagus consists of striated skeletal muscle. The lower third consists of smooth muscle and the medial third contains both types of muscle tissue. Between inner and outer layer, the autonomic nerve plexus is localized (plexus myentericus Auerbachii).
Tunica adventitia, tunica serosa
Serosa covers only abdominal part of esophagus. The rest of esophageal tube is covered by adventitia.
Histological slide of an esophagus is often confused with vagina. Esophagus contains glands, more fibroelastic connective tissue and its tunica muscularis is distinctly divided into two layers.
Stomach
The wall of stomach resembles the general organization of alimentary canal except a few differences.
Tunica mucosa
Mucosa forms foveolae gastricae – gastric pits. These are deep crypts lined by epithelium. Several (3-7) tubular gastric glands (glandulae gastricae). Glandulae gastricae extend from the bottom of gastric pits through lamina propria toward submucosa. Gastric mucosa (including the gastric pits) is lined by simple columnar epithelium with secretory function. Surface mucous cells produce mucus onto the surface of mucosa. This mucus protects and lubricates the mucosa.
Glandulae gastricae
In the glandular lining are found chief cells, parietal cells, mucous neck cells, undifferentiated stem cells and enteroendocrine cells.
1) Chief cells
The chief cells produce proenzymes which are later converted into active forms of digestive enzymes (pepsin, lipase). they are found in basal portions of glands.
2) Parietal cells
Parietal cells cause the low pH of gastric juice and produce intrinsic factor (glycoprotein necessary for absorption of vitamin B12 in terminal ileum). They are large with centrally located nuclei and eosinophilic cytoplasm.
3) Mucous neck cells
Mucous neck cells produce mucin stored in mucinogen granules in apical portion of these cells. The flattened nuclei are localized in the basal portion of cells.
4) Stem cells (undifferentiated cells)
They differentiate into other cellular types present in this area.
5) Enteroendocrine cells
Entero-endocrine cells are present mainly in corpus and fundus of stomach. Their products affect the motility of smooth muscle tissue in stomach and secretion of gastric juice by paracrine signalization. Their products involve gastrin produced by G-cells, somatostatin produced by D-cells and histamine produced by enterochromaffin cells.
Morphologically, we distinguish:
1) Cardiac glands
Cardiac glands are simple or rarely branched, widen. Mucous cells are present predominantly, parietal and chief cells are present in small number. Gastric pits are shallow.
2) Proper gastric glands (gll. gastricae propriae)
Proper gastric glands are found in corpus and fundus of stomach. Mostly are simple tubular with narrowed necks which empty into the gastric pits. Gastric pits are deeper in fundus and corpus than in cardia. In these glands, most of chief cells and parietal cells are found.
3) Pyloric glands (gll. pyloricae)
Gastric pits are deep, are present predominantly mucous cells and enteroendocrine cells (mainly G-cells).
Lamina propria mucosae is extended between glands and contains lymphatic tissue (folliculi lymphatici gastrici).
Tunica submucosa
There are no differences from general organization of alimentary canal.
Tunica muscularis
There are distinguished three muscular layers, from the inner surface outwards are they as follows: oblique, circular and longitudinal. Circular layer is significantly thicker in area of antrum pyloricum and forms here the pyloric sphincter. .
Tunica serosa
It is layer of visceral peritoneum and covers almost entire surface of stomach except the area of small and greater curvature where the omentum inserts.
Small intestine
the small intestine is divided into three parts – duodenum, jejunum and ileum. the wall of small intestine is composed of typical layers of alimentary canal. Mucosa of small intestine forms circular folds – plicae circulares Kerkringi. These folds are formed by mucosa and submucosa. They are most predominant in jejunum.
Tunica mucosa
The mucosal projections (consisting of epithelium and lamina propria mucosae) called intestinal villi (villi intestinales) are typical for small intestine mucosa. The simple tubular intestinal glands (glands of Lieberkühn) empty into the space between villi.
The surface of intestinal villi is covered by simple columnar epithelium with enterocytes and goblet cells. Aggregation of lymphatic tissue (MALT, mucosa associated lymphoid tissue) is present mostly in lamina propria but it can extend to the submucosa. The term MALT describes the lymphatic follicles covered by enterocytes with M-cells. M-cells (microfold cells) are specialized antigen-presenting cells which phagocyte various antigens and present it for immune cells localized below in lymphatic follicles.
Enterocytes possess numerous microvilli providing increase of cellular surface. On the surface of microvilli is glycoprotein complex called glycocalyx containing digestive enzymes. The complex of microvilli is called the brush border.
The goblet cells are unicellular mucous glands dispersed between enterocytes in intestinal mucosa.
Glands of Lieberkühn are intestinal crypts which empty into the mucosal surface. They contain columnar enterocytes, mucous cells, Paneth cells, stem cells and enteroendocrine cells. Paneth cells synthesize antibacterial enzyme lysozyme and other defensive proteins.
Enteroendocrine cells produce biologically active proteins e.g. gastrin, cholecystokinin and secretin.
Folliculi lymphatici solitarii are dispersed along the intestinal mucosa and aborally they increase in number. Aggregations of lymphatic tissue in the mucosa of intestine are called Peyer’s patches and they are most predominant in ileum. They measure about 2-10 cm in length. Above these accumulation of lymph tissue are villi less numerous or completely missing.
Muscularis mucosae consists of two layers of smooth muscle – outer longitudinal and inner circular.
Tunica submucosa
It is composed of loose collagenous connective tissue with blood and lymphatic vessels and nerves. In duodenum are characteristic submucosal Brunner’s glands lined by simple columnar epithelium. They are most predominant in pyloric area and their number decreases aborally. They disappear in duodenojejunal junction. Brunner’s glands are branched tubuloalveolar mucous glands producing alkaline secretion which participates in neutralization of acidic gastric chymus (together with pancreatic juice).
Tunica muscularis
Consists of thin outer longitudinal and thick inner circular layer.
Tunica serosa
Is a layer of loose connective tissue covered by mesothelium. The retroperitoneal part of duodenum is surrounded by adventitia.
Large intestine
Layers of the wall of large intestine differ in several aspects from general organization of alimentary canal:
1) Mucosa lacks circular folds (plicae circulares Kerkringi) and villi (villi intestinales)
2) Crypts of Lieberkühn are more often, longer and deeper. They are lined with simple columnar epithelium containing numerous goblet cells, resorptive colonocytes and small number of entero-endocrine cells
3) Except appendix the large intestine lacks Paneth cells.
Tunica mucosa
Lamina propria is very rich in lymphatic follicles which often extend into submucosa. Lymphatic follicles are most numerous in caecum, appendix and rectum. Lamina muscularis mucosae is composed of longitudinal and circular layer (it is similar to the small intestine).
Tunica submucosa
It has similar structure as the submucosa of small intestine.
Tunica muscularis
Tunica muscularis is composed of outer longitudinal and inner circular smooth muscle layer. The longitudinal layer is macroscopically thickened into three longitudinal belts – pásy – teniae coli. Circular layer is thicker in area of rectum and in area of anal canal creates the inner anal sphincter.
Tunica serosa
Tunica serosa creates little pockets filled with adipose tissue – appendices epiploicae.
Exocrine pancreas
Pancreas consists of exocrine and endocrine parts. Double function is divided into two structurally different compartments. Exocrine pancreas involves the whole organ but endocrine part is represented by dispersed accumulation of cells called islet of Langerhans.
Exocrine pancreas is serous gland often confused with parotid gland in histological slides. It is branched acinar gland composed of serous pyramidal-shaped cells with basophilic cytoplasm (basophilia is caused by prominent rough endoplasmic reticulum). Apical portion of cell contains large amount of zymogen granules staining with eosin. Granules contain digestive enzymes in inactive form.
Each acinus empty by intercalated duct lined by one layer of flattened cells which continue into the centre of acinus and thus are called centroacinar. Intercalated ducts are short and continue into interlobular collecting ducts. Pancreas lacks striated ducts.
Subchapter Author: Lucie Nováková and Bětka Blanková